A young woman presented to the hospital in the end of her second trimester of pregnancy. She had been vomiting for about 3 weeks, with a “mass” that comes and goes in her upper abdomen. When I discussed her condition with one of the nurses, he told me that he remembered the last time she was in the hospital a couple years ago (prior medical records could not be found). She was in her late 2nd trimester of pregnancy, but she continued vomiting until finally her baby was prematurely delievered and died. The patient herself stopped vomiting, until this time when she was at the same stage of pregnancy once again.
As I examined the patient, I could see that the top of her uterus was higher than her umbilicus. However, between the uterus and the ribcage, a peculiar thing could be seen. A firm swelling would grow in the left upper quadrant, then sweep across to the right side. This process was painful for the patient. It would then disappear for a few minutes, before becoming visible once again. The rest of the abdominal exam was normal.
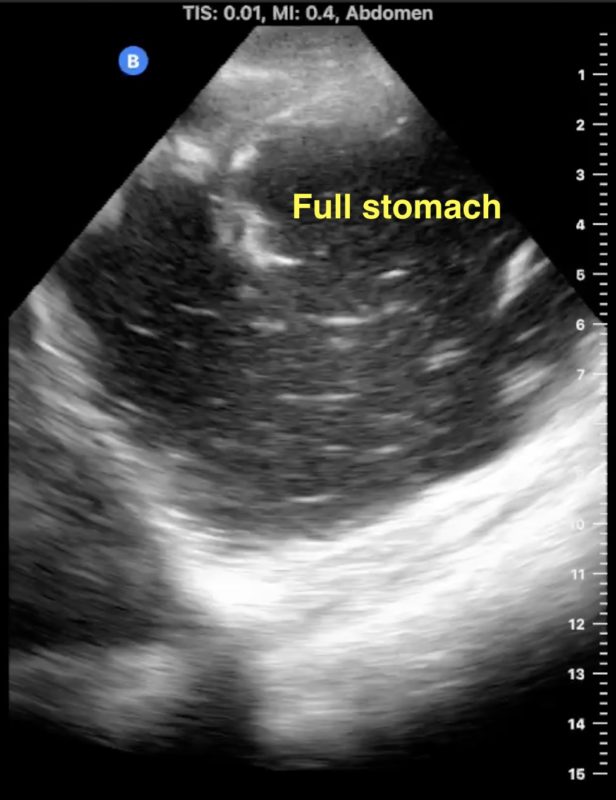
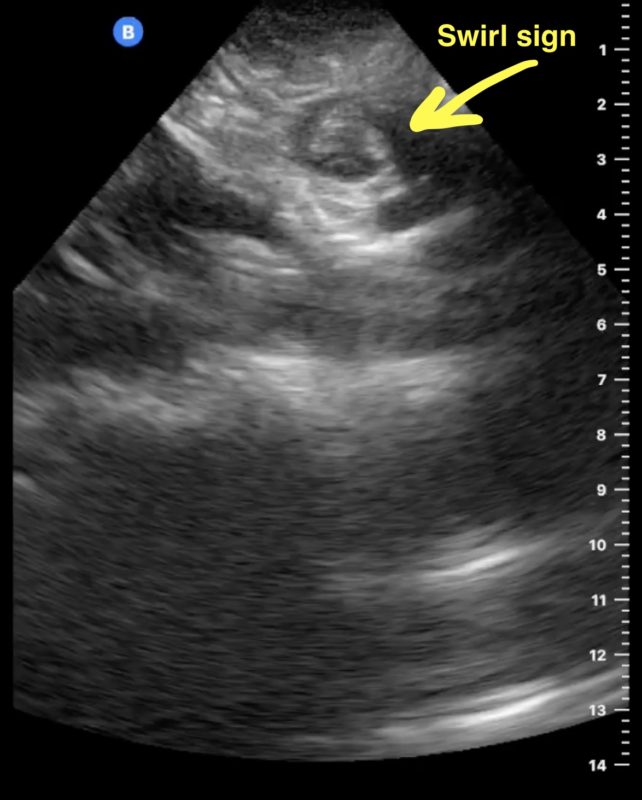
On ultrasound, the stomach was hugely dilated. It was full of fluid seen swishing back and forth. The movements seen through the abdominal wall were also noted as peristalsis on the ultrasound. The stomach could be seen transitioning into a very dilated duodenum. The transition from the duodenum into the jejunum was difficult to decipher between the large stomach and the gravid uterus. One peculiar area on ultrasound appeared to show a swirl of tissue – a “swirl” sign which sometimes signifies a twisting of the intestines causing a bowel obstruction.
We placed a nasogastric tube to decompress her stomach. Over the next 12 hours, 4 liters of fluid drained out of her stomach. The next day, she said she felt much better. She had been walking around and her bowels were even moving well. We clamped the tube, thinking maybe it was only a partial obstruction. She felt OK for the first day as she started to take in water and porridge again. However, when we rechecked with the ultrasound, her stomach was becoming dilated once again.
I struggled with the decision to take her to the operating room. I knew that operating on a pregnant woman could produce too much stress on her body and force her into premature labor. I also knew that if the patient wasn’t able to get nutrition in her body, her baby also would not get the needed nutrition to grow. After much prayer and preparation, I took her to the operating room. When I entered the abdomen, I realized that the appendix was staring at me from the left upper quadrant, instead of being in its normal position in the right lower quadrant. As I eviscerated the intestines (pulled them out of the abdomen) they were severely twisted, but not completely obstructed. I untwisted the bowel and confirmed what I had even conjectured while doing my ultrasounds – the patient had a malrotation and midgut volvulus of the intestines.

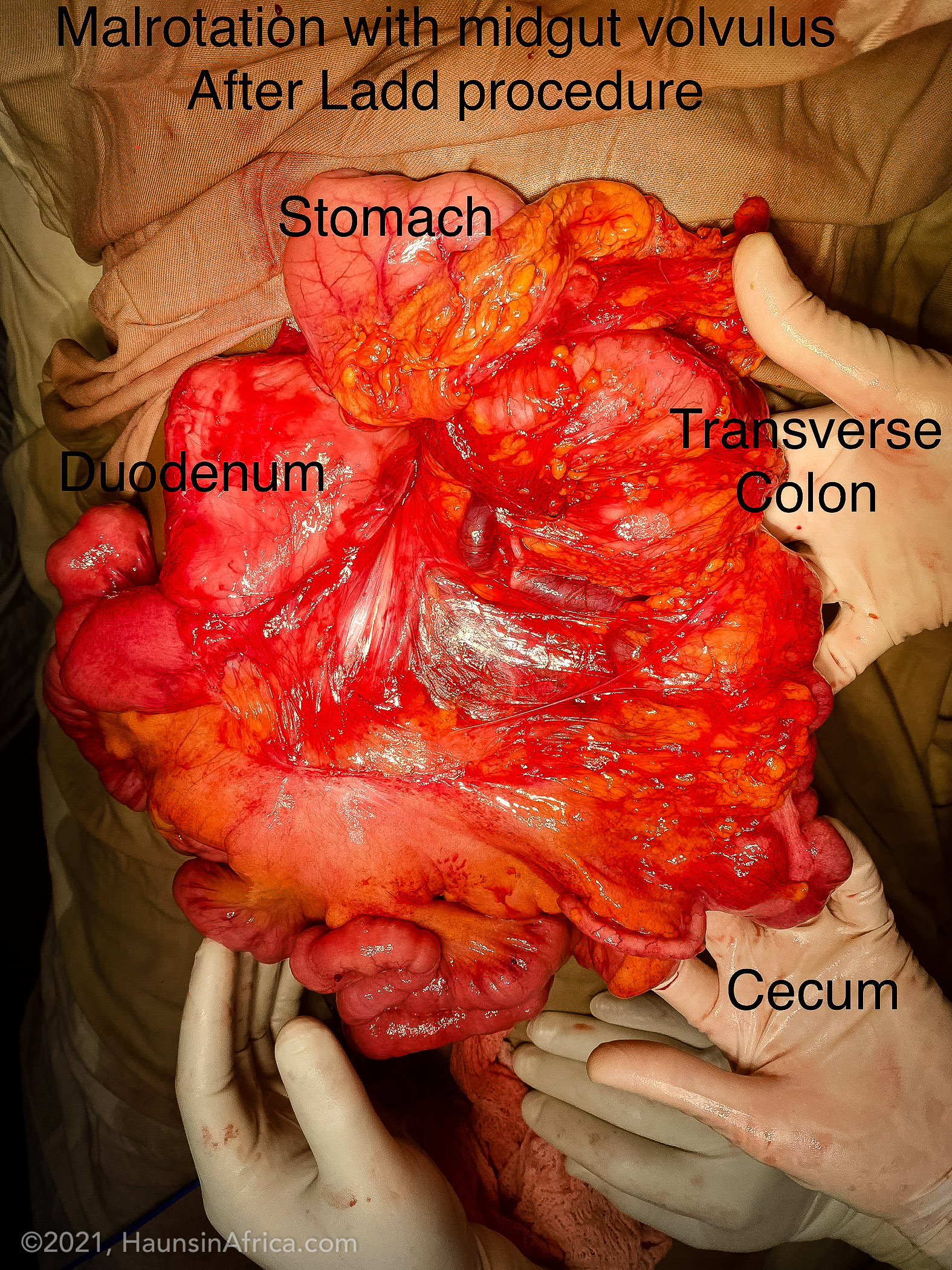
At some point, when the patient was still a fetus in her own mother’s womb, her intestines had not correctly positioned themselves within the abdomen. This “malrotation” allows for bands of scar tissue to be created between various structures in the abdomen but also makes it easier for the intestines to twist – especially when a gravid uterus is pushing up on them.
The treatment for malrotation is a procedure called the “Ladd procedure.” First, the intestines have to be untwisted in a counter-clockwise direction. Secondly, the scar tissue between structures (especially the cecum and the duodenum) are divided. Thirdly, the mesentery which carries the blood supply for the intestines must be broadened – dividing the aberrant scar tissue which is also present there. Fourthly, an appendectomy is performed (because appendicitis is difficult to correctly diagnose when the cecum is far from its normal position!) Finally, the bowel is placed back into the abdomen with all the small intestine on the right side and the colon on the left, with the cecum in the left upper quadrant.
For my patient, having a gravid uterus seemed very convenient to helping the bowel stay in the correct orientation as I placed the small intestines on the right of the uterus and all of the colon on the left. The body will create new scar tissue to hold the bowels in the correct place.
By the next day, she could tell that her intestinal path was now open again. By postoperative day 2, she was passing gas and having bowel movements and she was no longer vomiting. She continued to improve daily.
As for her baby, ultrasounds performed in the hours after surgery showed that the baby was alive and kicking. Unfortunately, the baby passed a couple weeks later but the mother continues to do well.